Pain- Decoding the body's warning system
- Si Hyeong Park
- Jan 6, 2024
- 4 min read
Updated: Jan 8, 2024
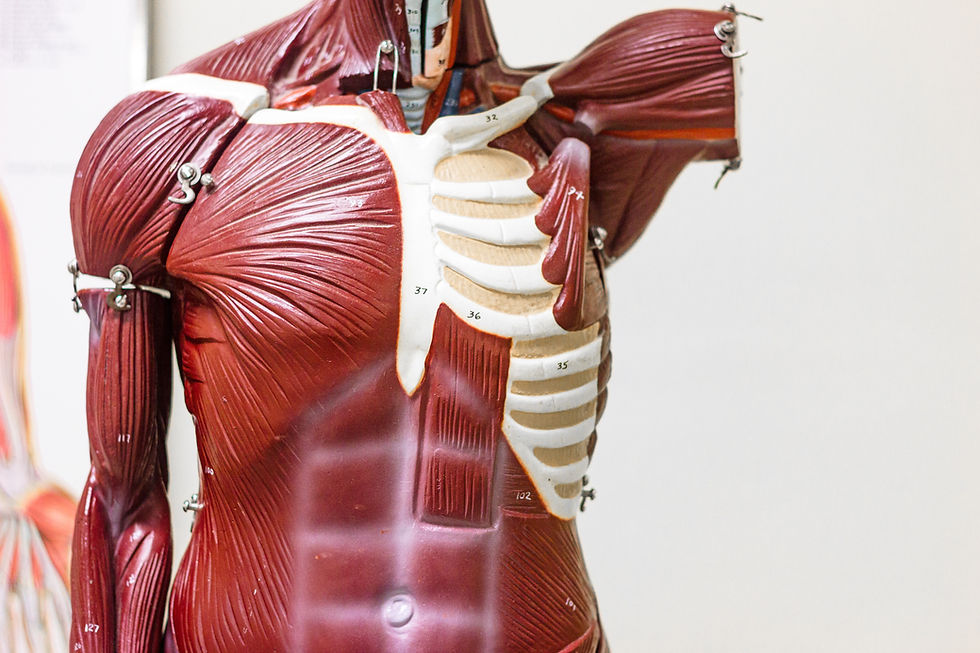
Stubbing your toe. Hitting your head. Breaking a leg. These all have at least one thing in common: pain. It’s an inevitable feeling that almost all of us have experienced, but also one that we may not understand very well. In this exploration of the pain mechanism, we’ll be delving into what pain actually is and how different individuals interpret and ‘feel’ pain, along with the real world example of spice.
Pain is your brain notifying you of danger. When you are exposed to harmful or potentially dangerous environments, specialised pain-sensing nerves called nociceptors sense this and send threat signals to your brain. This part is normally associated with an unpleasant feeling known as pain. Chemical messengers called neurotransmitters carry all of these signals, and when your brain receives these danger signals it then decides a response. This response could decrease the painful feeling you are experiencing, by releasing natural painkillers called endorphins. However, it could also choose to increase the pain felt instead, by releasing neurotransmitters that will enhance the pain. In short, your body detects the danger, tells your brain about the danger, and then it creates a response. Our bodies use pain as a way to protect ourselves. For example, if you have an injury that’s still healing, you will experience pain around the area when you use it, as your body wants you to let it heal.
The pain you experience directly from an injury is called acute pain, which signals a specific danger, and goes away after your body heals. However, sometimes pain persists for a long time, even when there’s nothing the body wants to protect or warn you about. When this pain persists for longer than 3 months despite treatment, it is called chronic pain; your body continues to send out pain signals, even when there is seemingly nothing wrong. When neurotransmitters continue to be sent out, it can make the pathway the signals travel through very sensitive, and thus amplify the pain more. This is why you might experience pain even after your injury has fully healed.
Within the healthcare sector, gauging the amount of pain a patient is experiencing is often a difficult task. This is particularly true for some patients, such as younger children, who may not have the communication skills to explain what the pain feels like. Furthermore, there are many psychological factors that may make a patient give the doctor an inaccurate self-report, such as having a fear of hospitals or medicine, or feeling embarrassed about their injury. As a result, this could compromise a doctor’s ability to make an accurate diagnosis. This is why it is vital that hospitals are perceived as safe and comfortable environments in order to reduce the possibility of inaccurate reporting of pain, which would .
However, pain is not just associated with injuries, it is also involved within our diets. Capsaicin, a chemical found in chillies, causes pain to stem from spiciness. Our mouths contain a vast number of nociceptors, with the nociceptor ‘TRPV1’ specifically detecting high temperatures. It is interesting to note that capsaicin also activates TRPV1 nociceptors, resulting in the familiar burning sensation, similar to that of when we burn ourselves. But why do so many people enjoy this burning sensation? As previously learnt, once the brain receives danger signals, it creates a response. With spicy food, our brain detects the pain from the nociceptors in our mouths and responds by releasing endorphins. Endorphins are pleasure causing hormones which seemingly ‘eliminate’ the pain. This results in a ‘high’ that some experience, which you can compare to what you might get after running. This explains why some people associate spiciness with happiness, resulting in a multitude of people enjoying spicy food.
Everyone interprets pain differently, with some having a lower tolerance and others having a higher one. Recent research has shown this to be as a result of varying numbers of neurotransmitters amongst individuals, so those with more will tend to feel more pain when exposed to the same stimuli compared to someone else with lower numbers of neurotransmitters. In terms of spiciness, those with more TRPV1 receptors will have a greater burning feeling in their mouth as a result of the spice, and thus will find the food spicier. Another factor that shapes how we tolerate pain and spice is past experiences. If you have been exposed to the same stimuli multiple times, you begin to build a tolerance, and over time it will not feel as painful. Therefore, children tend to have a lower pain and spice tolerance as they are likely to not have experienced as many stimuli. This explains why babies and toddlers also cry more frequently from pain.
In conclusion, as we have learnt about how the body processes pain along with its involvement in spice, it is evident that it is a complex and multifaceted experience. Despite being ubiquitous, pain is a different experience for everyone and depends on a myriad of factors. It is your body warning you of a potential danger, but we also know that in cases of chronic pain and other scenarios, it doesn’t always serve this purpose. Our knowledge of pain is still a work in progress and there is still vast amounts to learn about this complex mechanism. Nevertheless, as time and technology progresses, our understanding of it continues to grow, promising future discoveries and development for the study of pain science.