The Resurgence of Psychedelic Therapy: A New Era in Mental Health Treatment
- Anish Chatterjee
- May 6, 2024
- 3 min read
Serotonergic hallucinogens, commonly known as psychedelics, are a class of drug with powerful psychoactive properties that alter the senses, cognitive processes and mood of an individual. The usage of psychedelic substances is prevalent in human history. The first record of such dates back 6,000 years, with cave drawings depicting the naturally occurring compound Psilocybin found in mushrooms. Psilocybin has similar effects to lysergic acid diethylamide (LSD) which was synthesised by the Swiss chemist Albert Hoffman in 1938. banning of psychedelic research in the mid-20th century stifled scientific exploration until recent decades, but we are now entering a psychedelic renaissance, with shifting perspectives driving a renewed interest in their therapeutic potential.
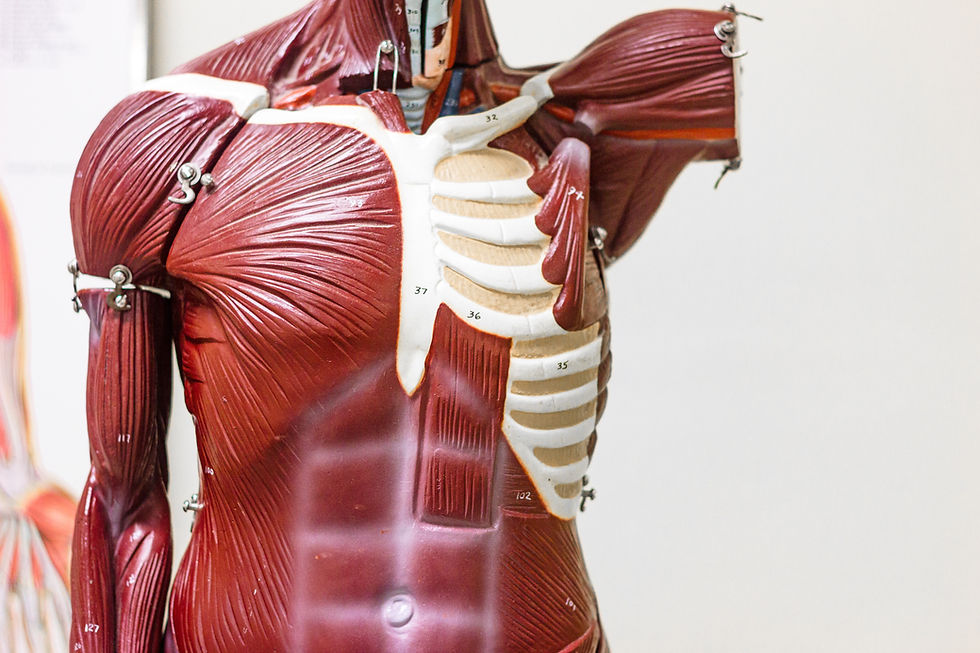
To unravel the benefits of psychedelics, ongoing research by scientists are investigating the brain chemistry and mechanisms through which these substances exert their effects. So far, we know that naturally occurring hallucinogens (such as Psilocybin, LSD, and DMT) stimulate a specific serotonin receptor in neural brain cells called the 5-hydroxytryptamine 2A receptor. These hallucinogens effectively copy the action of the chemical messenger serotonin by binding to the serotonin 2a receptor, changing its ‘shape’, internal conditions and consequently its neural behaviour by increasing the neurone’s excitability (excitability is the neurone’s readiness to produce electrical impulses in response to stimulation).
Serotonin 2A receptors are primarily expressed on an important type of neurone in the brain known as an excitatory pyramidal neurone, particularly in layer 5 of the cortex, a deep layer essential for integrating and processing information. Hallucinogens stimulate serotonin 2A receptors, inducing excitation in these layer 5 pyramidal neurones, altering their firing patterns and disrupting their synchronisation with electrical activity. This disruption, observed through neuroimaging techniques, results in a disorganised pattern of brain activity across different frequencies. This disorganisation leads to the characteristic changes in perception and consciousness associated with hallucinogenic experiences.
This knowledge prompted an investigation into psychedelic-assisted therapy and its implications for revolutionising psychiatric treatment. Researchers at Imperial College London conducted a trial in which they tested the therapeutic potential of the psychedelic compound psilocybin, comparing it to a major antidepressant drug (escitalopram) in patients with moderate-to-severe depression. Patients underwent a six-week course and researchers concluded that while in both groups’ depression scores were lowered, the reductions happened more rapidly and at a greater magnitude in the psilocybin group than the antidepressant drug. With psilocybin, patients showed clear improvements in their ability to experience pleasure and convey emotions, experienced significant decreases in anxiety and suicidal thoughts, and reported heightened feelings of well-being.
A significant reduction in depression scores was seen in 70% of patients in the psilocybin group, compared with 48% in the escitalopram group. Remission of symptoms was seen in 57% of the psilocybin group, compared with just 28% in the escitalopram group. While the trial showcasing psilocybin's efficacy in depression treatment is promising, the trial’s small sample size (59) and the absence of placebo testing limit definitive conclusions. However, these initial findings highlight the potential of psychedelic-assisted therapy, suggesting possible further research will be necessary to better understand and perhaps someday legally license psilocybin as a medicine.
A similar case of psycho-assisted therapy was in the treatment of Post-Traumatic Stress Disorder (PTSD) through 3,4-Methylenedioxymethamphetamine (MDMA). MDMA is quite different than psilocybin as it is a synthetic psychedelic, and its psychedelic properties were not discovered until around 60 years after its creation. It was not until the 21st century that MDMA was studied as a potential treatment for PTSD. Studies have highlighted MDMA's ability to enhance prosocial behaviour, emotional empathy, and feelings of openness and trust, alongside its neurobiological effects on reducing fear and anxiety-related brain activity while promoting higher-level thinking in regions like the frontal cortex. This is particularly beneficial in patients suffering from PTSD as they frequently have dysfunctional frontal cortex activity. Researchers at the University of California performed a recent study in which they used MDMA as a treatment for PTSD in 104 participants. Results showed that combining MDMA with talk therapy significantly reduced symptoms, with 86.5% experiencing improvements and 71% no longer meeting PTSD criteria. These results highlight the therapy's effectiveness (especially when compared to the placebo group) and therefore the potential for MDMA-assisted therapy to become a transformative intervention for PTSD treatment.
The future of psychedelics in medicine introduces a new era of innovation and potential. With ongoing research revealing their efficacy in treating a myriad of diseases, from mental health conditions to chronic physical illnesses, these substances hold promise for transforming healthcare. As we continue to explore their applications and benefits, psychedelics could revolutionise medicine, saving lives and contributing significantly to global well-being.